Laryngo-tracheo-bronchoscopy Team Brief - Patient 1
Paediatric ENT SurgeryUse this resource in conjunction with your real-world training

Experience Summary
Laryngo-tracheo-bronchoscopy (LTB) is a diagnostic/therapeutic procedure used in the evaluation of the upper and lower airway in children with stridor, suspected airway obstruction, congenital anomalies, foreign body aspiration, or persistent respiratory symptoms. In this 360-degree video observe the multidisciplinary team performing a team brief for a theatre list of LTBs.
Clinical Context
Given the shared airway, the child’s physiological vulnerability, and the potential for rapid deterioration, conducting a structured team brief is essential to optimize safety and procedural success.
The paediatric airway differs significantly from the adult airway in terms of size, anatomical proportions, and reactivity, making airway interventions more technically challenging and less forgiving. Children desaturate more quickly during apnoea, have less oxygen reserve, and are more prone to laryngospasm, bronchospasm, or complete obstruction. These risks are amplified during LTB, where dynamic airway collapse, obstruction, or bleeding may occur. The team brief provides a critical opportunity to align all team members - anaesthetists, ENT surgeons, and theatre staff - on the procedural plan, roles, equipment, and contingencies.
During the brief, essential details are shared, including the child’s medical history, presenting airway symptoms, previous anaesthetic or surgical interventions, imaging findings, and potential airway difficulties. Anaesthetic planning is discussed in depth: whether the procedure will be performed under spontaneous or controlled ventilation, the type of induction (inhalational vs. intravenous), and the approach to airway maintenance (e.g. facemask, laryngeal mask airway, endotracheal tube, or apnoeic oxygenation). The team should also prepare for rapid transition between techniques and anticipate complications like desaturation or obstruction.
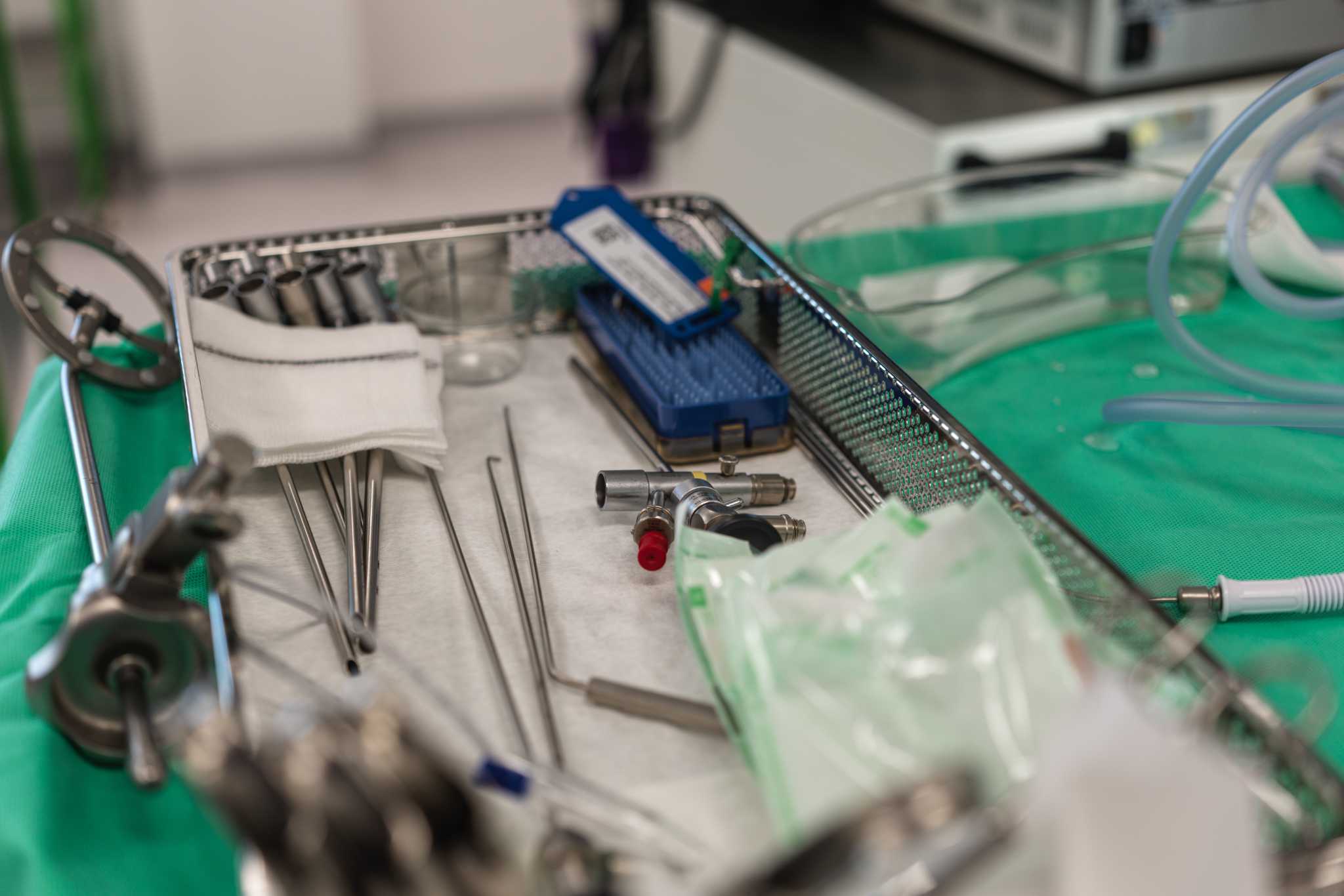
The surgical team outlines procedural steps, required instrumentation (e.g. rigid bronchoscope, Hopkins rod, suction), and specific objectives (biopsy, foreign body removal, dilatation). Availability and readiness of backup airway equipment (e.g. jet ventilation, tracheostomy set) and emergency drugs must be confirmed.
Importantly, a shared mental model of the sequence is developed, with clearly assigned roles and crisis checklists, if applicable. Open communication, mutual respect, and the presence of a named team leader foster cohesion and rapid decision-making.
Learning Objectives
- Understand the importance of team briefing prior to LTBs .
- Understand some of the indications for performing LTBs in children .
- Understand the various roles of the MDT in LTBs .
