Tonsillectomy - Procedure
Paediatric ENT SurgeryUse this resource in conjunction with your real-world training
Experience Summary
In this 360-degree video, observe the surgical procedure of a paediatric tonsillectomy on a real patient.
Clinical Context
A tonsillectomy is the surgical removal of the palatine tonsils; often this is done together with adenoidectomy (adenotonsillectomy) in paediatric patients. The procedure is among the most common childhood surgeries and is considered when the tonsils cause significant problems that are not adequately controlled by medical therapy.
Indications:
- Recurrent tonsillitis / sore throats: frequent episodes of bacterial tonsillitis (e.g., meeting criteria such as the “Paradise” criteria: for example seven or more episodes in one year, or five or more per year over two years, or three or more per year over three years).
- Sleep-disordered breathing / obstructive sleep apnoea (OSA): when tonsil and/or adenoid hypertrophy obstruct the airway, causing snoring, disturbed sleep, behavioural or growth issues.
- Severe complications: peritonsillar abscess not responsive to drainage/medical management; rare but serious issues like febrile seizures triggered by tonsillitis or tonsillar disease suggestive of malignancy (e.g. unilateral enlargement).
These interventions are weighed against the risks, as tonsillectomy has potential complications: bleeding (intra- and post-operatively), anaesthetic risk, pain, swallowing difficulties, dehydration, etc. Moreover, many guidelines emphasise that not all children with sore throats or tonsillitis are good candidates; quality of life, severity, frequency, response to medical therapy, and comorbidities must be considered.
Procedural Steps
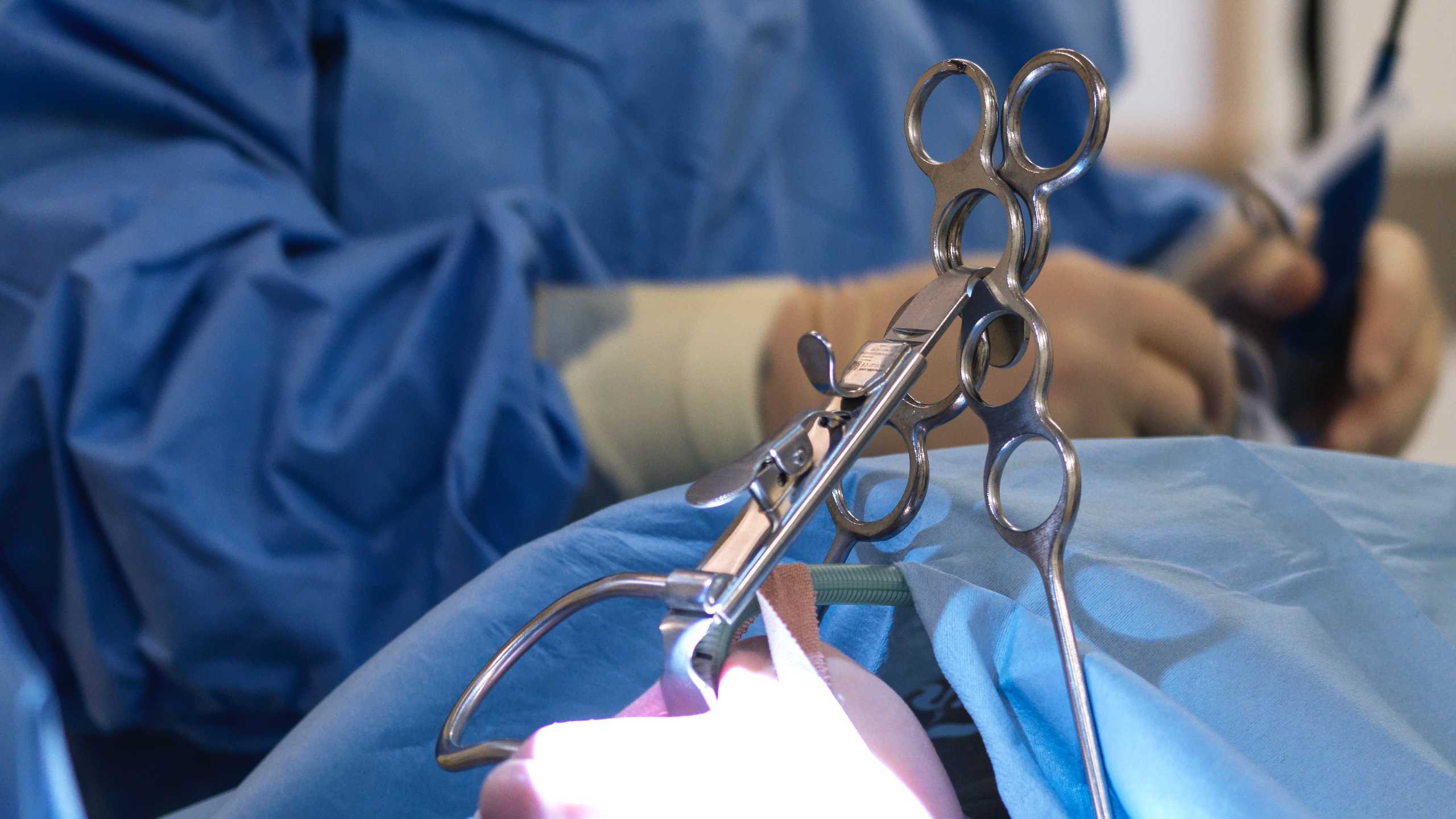
After general anaesthesia is induced and the airway is secured, the child is positioned supine with a shoulder roll to extend the neck. A mouth gag—commonly a Boyle-Davis gag—is inserted carefully to provide exposure while avoiding dental or soft-tissue trauma. The gag is attached to a suspension system to maintain stability throughout the procedure. The tonsils are then inspected, and the surgical field is illuminated. Techniques such as cold steel dissection, monopolar or bipolar diathermy, coblation, or microdebrider-assisted dissection may be used depending on surgeon preference. Regardless of the modality, the procedure typically begins by grasping the tonsil with a forceps and making an incision along the mucosa of the anterior tonsillar pillar. The tonsil is dissected along its natural capsular plane, freeing it from the surrounding musculature.
Once the tonsil is removed, meticulous haemostasis is essential due to the rich vascular supply of the tonsillar fossae. Surgeons may use bipolar cautery, suction diathermy, or ligatures to control bleeding. The process is repeated on the contralateral side following the same steps. After both tonsils are excised and haemostasis is confirmed, the mouth gag is released slowly to ensure there is no airway obstruction or renewed bleeding. A final inspection of the oropharynx is performed, sometimes accompanied by gentle suctioning to clear secretions or blood. The patient is then handed back to the anaesthetic team for emergence and postoperative airway management. Smooth transition to recovery is essential, as the early postoperative period carries risks of laryngospasm, airway obstruction, and nausea.
Learning Outcomes
- Understand the indications for tonsillectomy in paediatric patients.
- Understand the procedural steps of a tonsillectomy.
- Observe a tonsillectomy being performed on a paediatric patient.
- Understand the key safety steps involved in a tonsillectomy.
External Resources