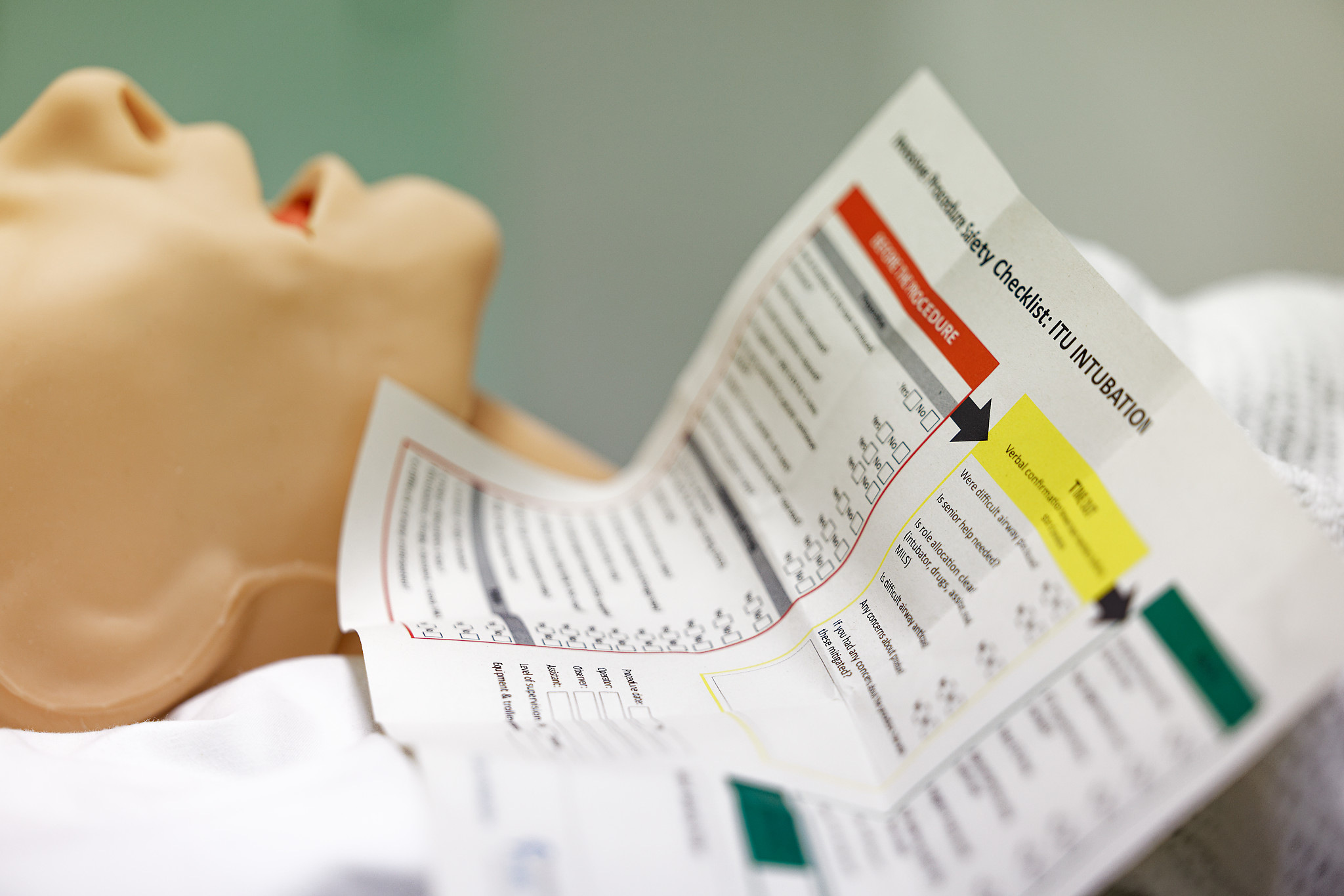
Rapid sequence induction (RSI) preparation outside the theatre
Outside-Theatre Checklists360 Video

Use this resource in conjunction with your real-world training
Share

Experience Summary
In this 360-degree video watch as the anaesthetic team performs a rapid sequence induction (RSI) checklist prior to performing the procedure.
RSI is a critical airway management technique used to rapidly induce unconsciousness and neuromuscular blockade in patients at high risk of aspiration. It is commonly employed in emergency settings where airway protection is urgently needed, such as in trauma, sepsis, or reduced consciousness. To ensure patient safety and maximise first-pass success, a structured pre-induction checklist and adherence to RSI steps are essential.
Clinical Context
A thorough preparation checklist includes the following components, often remembered using the mnemonic “SOAP ME”:
- S – Suction: Ensure suction is functional and within reach, with a Yankauer tip ready.
- O – Oxygen: Pre-oxygenate the patient with 100% oxygen for 3–5 minutes using a non-rebreather mask or bag-valve mask with a reservoir. In some cases, apnoeic oxygenation via nasal cannula is also applied.
- A – Airway Equipment: Prepare all airway tools including a working laryngoscope (with backup blades), endotracheal tubes (ETTs) of appropriate sizes, bougie or stylet, and alternative airway devices (e.g., supraglottic airway, video laryngoscope).
- P – Pharmacology: Draw up and label induction and paralytic agents. Common drugs include etomidate, ketamine, or propofol (induction) and suxamethonium or rocuronium (paralysis). Have emergency drugs like atropine and vasopressors ready.
- M – Monitoring: Attach ECG, pulse oximeter, non-invasive blood pressure, and capnography if available.
- E – Emergency Equipment: Ensure availability of a bag-valve mask, crash trolley, defibrillator, and backup airway plan (Plan B/C/D).
Steps of Performing RSI
- Preparation: Complete the checklist, brief the team, and assign roles (airway, drugs, cricoid pressure, documentation).
- Pre-oxygenation: Administer 100% oxygen for at least 3 minutes to increase oxygen reserves and reduce the risk of desaturation during apnea.
- Induction and Paralysis: Administer the induction agent, followed immediately by the neuromuscular blocker. Cricoid pressure may be applied if indicated, though its use is debated.
- No Ventilation: Avoid bag-mask ventilation unless desaturation occurs, to reduce aspiration risk.
- Intubation: Once paralysis is confirmed (usually after 45–60 seconds), proceed with laryngoscopy and intubation. Confirm tube placement with capnography, chest rise, and auscultation.
- Post-intubation Management: Secure the tube, resume ventilation, and start appropriate sedation and analgesia. Reassess airway, breathing, and circulation.
Learning Objectives
- Understand the rapid sequence induction process and safety critical measures.
- Understand the role of a safety checklist.
External Resources
